NightWatch
NightWatch is a multimodal wearable sensor that detects major nocturnal epileptic motor seizures, being¹:
- Tonic-Clonic seizures
- Tonic seizures (if cluster or prolonged)
- Myoclonic seizures (if cluster)
- Focal seizures (impaired awareness with hyperkinetic movements)
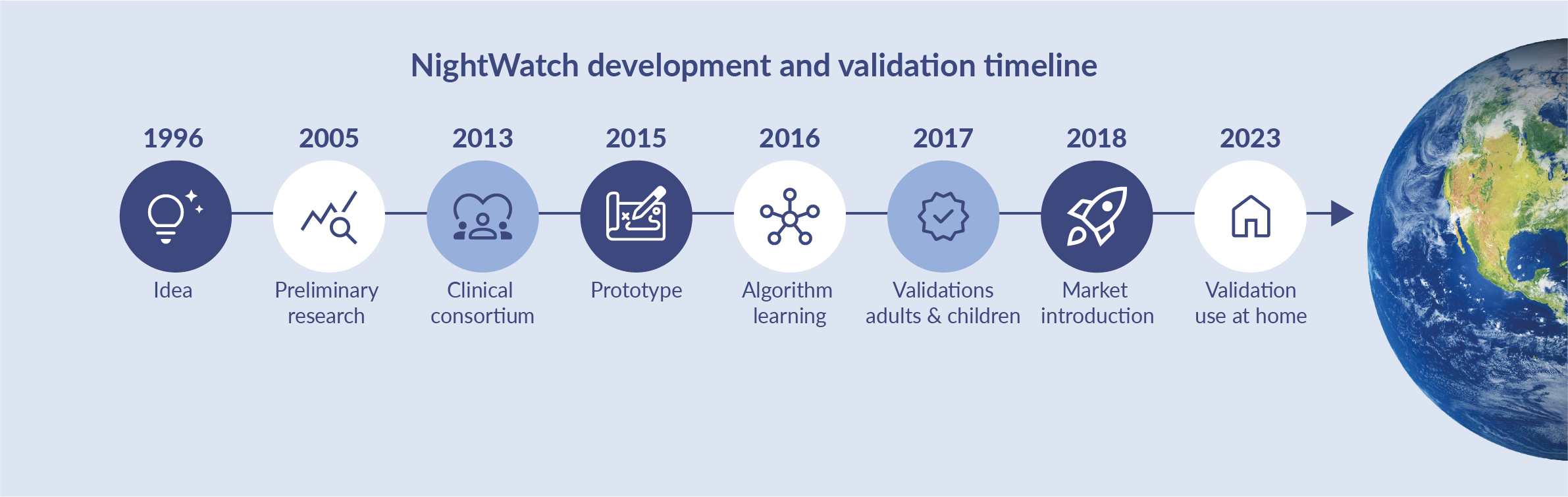
The clinical validation timeline
NightWatch was invented and developed by a consortium of Dutch neurologists, patient organisations, universities and hi-tech industries. Our joint mission is to reduce SUDEP (Sudden Unexpected Death in Epilepsy) patients and improve the quality of life for individuals with epilepsy and their caregivers.
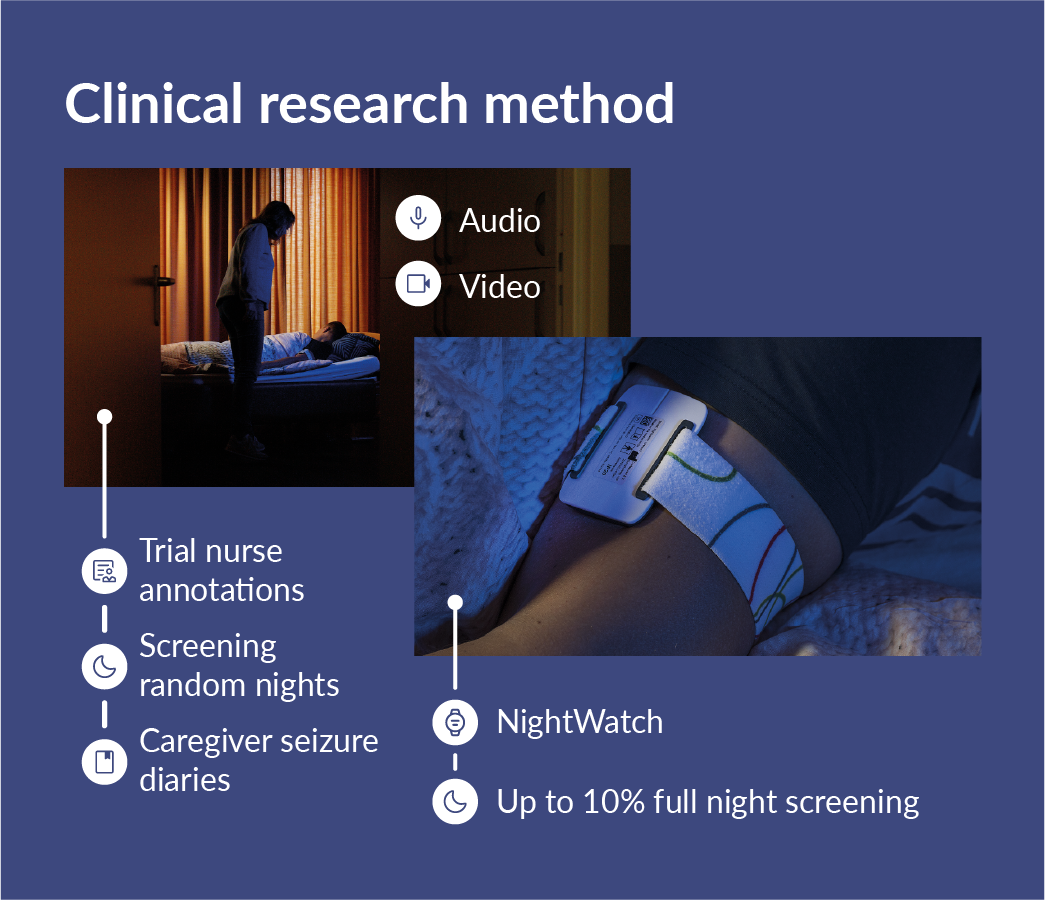
Study design
NightWatch has been validated in multiple video-controlled, prospective, multicenter, long-term trials. These trials involved trained trial nurses who used video and audio for annotation. The study design allowed for evaluating the device’s performance in a realistic home environment setting over an extended period. Various screening methods were applied to mitigate the bias of missing seizures due to the lack of continuous EEG supervision, which could inflate sensitivity. Firstly, caregivers were asked to keep track of all noticed seizures. Secondary automated seizure detection technologies, such as bed sensors and retrospective video detection, were also utilized. Finally, trial nurses screened 5%-10% of all video recordings to identify seizures.
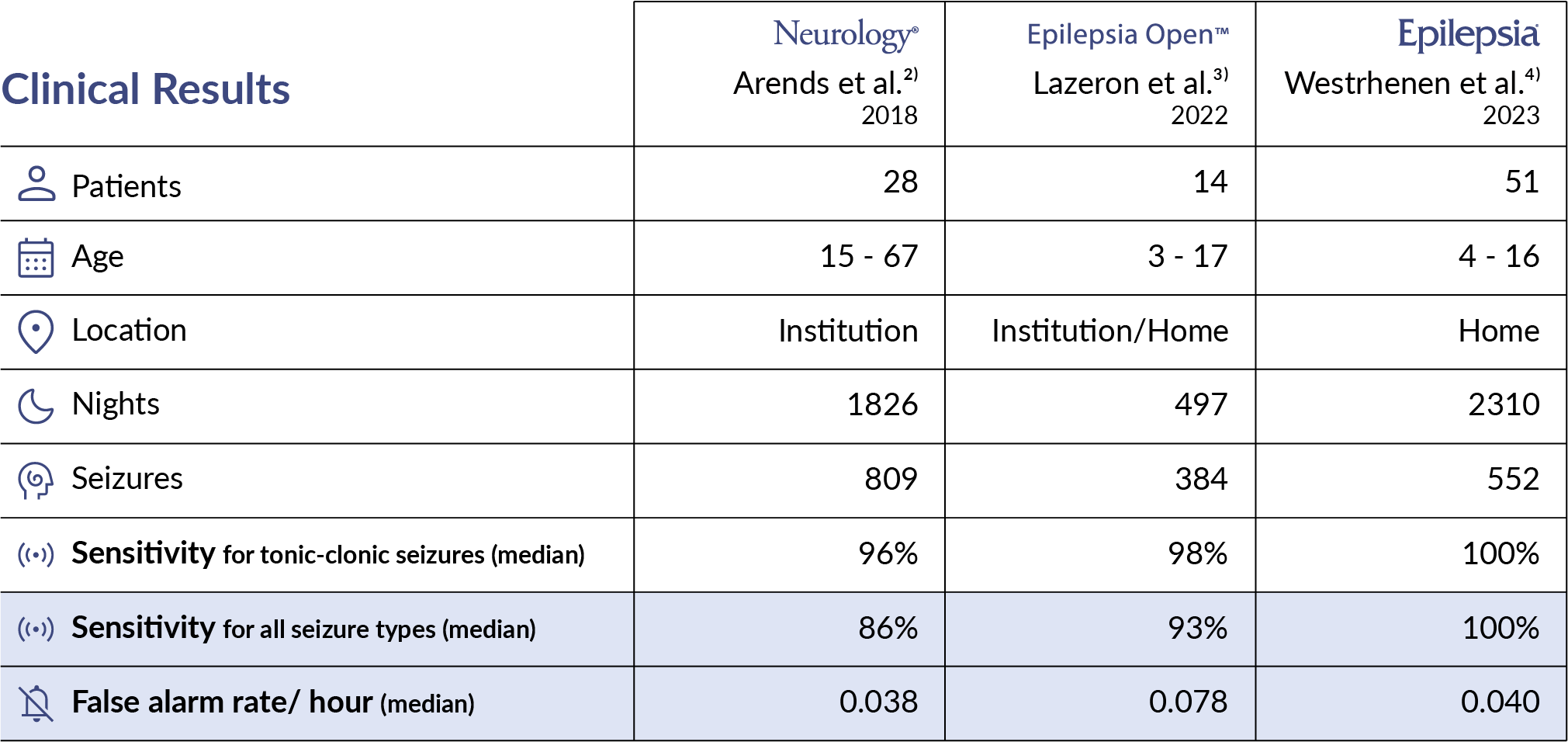
The effectiveness of NightWatch has been clinically evaluated in phase 3 and 4 prospective multicenter clinical trials over the last five years¹ ³ ⁴. The aggregated results are visualised below.
Primary outcomes
The table below illustrates the outcomes of the studies.
Secondary outcomes
Using NightWatch for two months showed a significant reduction in stress among parents compared to the two months before use⁵. This is indicated by the total Caregiver Strain Index (CSI) score of 8.0 vs 7.1; p=0.032.
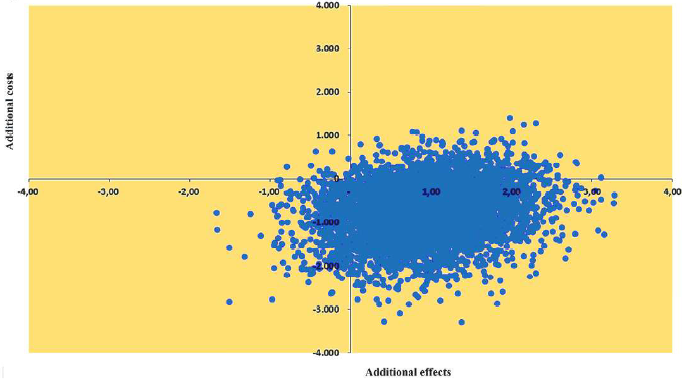
Using NightWatch for two months showed a calculated reduction of the cost of care by € 775 compared to the two months before use⁵. Moreover, the cost-effectiveness analysis for NightWatch reveals that 82% of the Incremental Cost-Effectiveness Ratios (ICERS) lie in the dominant southeast quadrant, indicating that NightWatch is less expensive and more effective than usual care.
Download the Economic evaluation of NightWatch for children with refractory epilepsy.
Why is the detection of nocturnal epileptic seizures important?
- 86% of nocturnal seizures happen unnoticed².
- Timely intervention at nocturnal seizures can decrease body injuries, status epilepticus and SUDEP².
- The unpredictability of seizure occurrence is distressing for patients and caregivers, contributes to social isolation, and decreases the quality of life².
NightWatch improves the safety of individuals with nocturnal epileptic motor seizures and reduces the stress of caregivers by alarming them during the occurrence of a nocturnal epileptic motor seizure. This enables caregivers to provide appropriate measures when required.
Cited literature
- Arends J, Thijs RD, Gutter T, Ungureanu C, Cluitmans P, van Dijk J, et al. Multimodal nocturnal seizure detection in a residential care setting: A long-term prospective trial, Neurology. 2018 Nov 20; 91(21):e2010-e2019. doi: 10.1212/WNL.0000000000006545
- Beniczky S, Wiebe S, Jeppesen J, Tatum WO, Brazdil M, Wang Y, et al. Automated seizure detection using wearable devices: A clinical practice guideline of the International League Against Epilepsy and the International Federation of Clinical Neurophysiology. Epilepsia. 2021 Mar; 62(3):632-646. doi: 10.1016/j.clinph.2020.12.009.
- Lazeron RHC, Thijs RD, Arends J, Gutter T, Cluitmans P, van Dijk J, et al. Multimodal nocturnal seizure detection: Do we need to adapt algorithms for children? Epilepsia. 2022; 7(3):406–13. doi: 10.1002/epi4.12618
- van Westrhenen A, Lazeron RHC, van Dijk JP, Leijten FSS, Thijs RD, the Dutch TeleEpilepsy Consortium. Multimodal nocturnal seizure detection in children with epilepsy: A prospective, multicenter, long‐term, in‐home trial. Epilepsia. 2023. doi: 10.1111/epi.17654
- Engelgeer A, van Westrhenen A, Thijs RD, Evers SMAA. An economic evaluation of the NightWatch for children with refractory epilepsy: Insight into the cost-effectiveness and cost-utility. Seizure. 2022;101:156–61. doi: 10.1016/j.seizure.2022.08.003
Literature list of other publications
- Zelano, J., Beniczky, S., Ryvlin, P., Surges, R., Tomson, T., & the ILAE SUDEP Task Force. (2023). Report of the ILAE SUDEP Task Force on national recommendations and practices around the world regarding the use of wearable seizure detection devices: A global survey. Epilepsia Open. doi.org/10.1002/epi4.12801
- Hadady L, Klivényi P, Fabó D, Beniczky S. Real-world user experience with seizure detection wearable devices in the home environment. Epilepsia. 2022;00:1–6. doi: 10.1111/epi.17189
- van Elmpt WJC, Nijsen TME, Griep PAM, Arends JBAM. A model of heart rate changes to detect seizures in severe epilepsy. Seizure. 2006;15(6):366–75. doi: 10.1016/j.seizure.2006.03.005
- Massé F, Penders J, Serteyn A, van Bussel M, Arends J. Miniaturized wireless ECG-monitor for real-time detection of epileptic seizures. WH’10. 2010 Oct; 111-117. doi: 10.1145/1921081.1921095
- Lamberts RJ, Thijs RD, Laffan A, Langan Y, Sander JW. Sudden unexpected death in epilepsy: People with nocturnal seizures may be at highest risk: Nocturnal Seizures as a Risk for SUDEP. Epilepsia. 2012;53(2):253–7. doi: 10.1111/j.1528-1167.2011.03360.x
- van Andel J, Leijten F, van Delden H, van Thiel G (2015) What Makes a Good Home-Based Nocturnal Seizure Detector? A Value Sensitive Design. PLoS ONE 10(4): e0121446. doi: 10.1371/journal.pone.0121446
- Arends JB, van Dorp J, van Hoek D, Kramer N, van Mierlo P, van der Vorst D, et al. Diagnostic accuracy of audio-based seizure detection in patients with severe epilepsy and an intellectual disability. Epilepsy Behav. 2016;62:180–5. doi: 10.1016/j.yebeh.2016.06.008
- van Andel J, Thijs RD, de Weerd A, Arends J, Leijten F. Non-EEG based ambulatory seizure detection designed for home use: What is available and how will it influence epilepsy care? Epilepsy Behav. 2016;57:82–9. doi: 10.1016/j.yebeh.2016.01.003
- van der Lende M, Cox FME, Visser GH, Sander JW, Thijs RD. Value of video monitoring for nocturnal seizure detection in a residential setting. Epilepsia. 2016;57(11):1748–53. doi: 10.1111/epi.13558
- van Andel J, Ungureanu C, Arends J, Tan F, Van Dijk J, Petkov G, et al. Multimodal, automated detection of nocturnal motor seizures at home: Is a reliable seizure detector feasible? Epilepsia Open. 2017;2(4):424–31. doi: 10.1002/epi4.12076
- Geertsema EE, Thijs RD, Gutter T, Vledder B, Arends JB, Leijten FS, et al. Automated video-based detection of nocturnal convulsive seizures in a residential care setting. Epilepsia. 2018;59:53–60. doi: 10.1111/epi.14050


